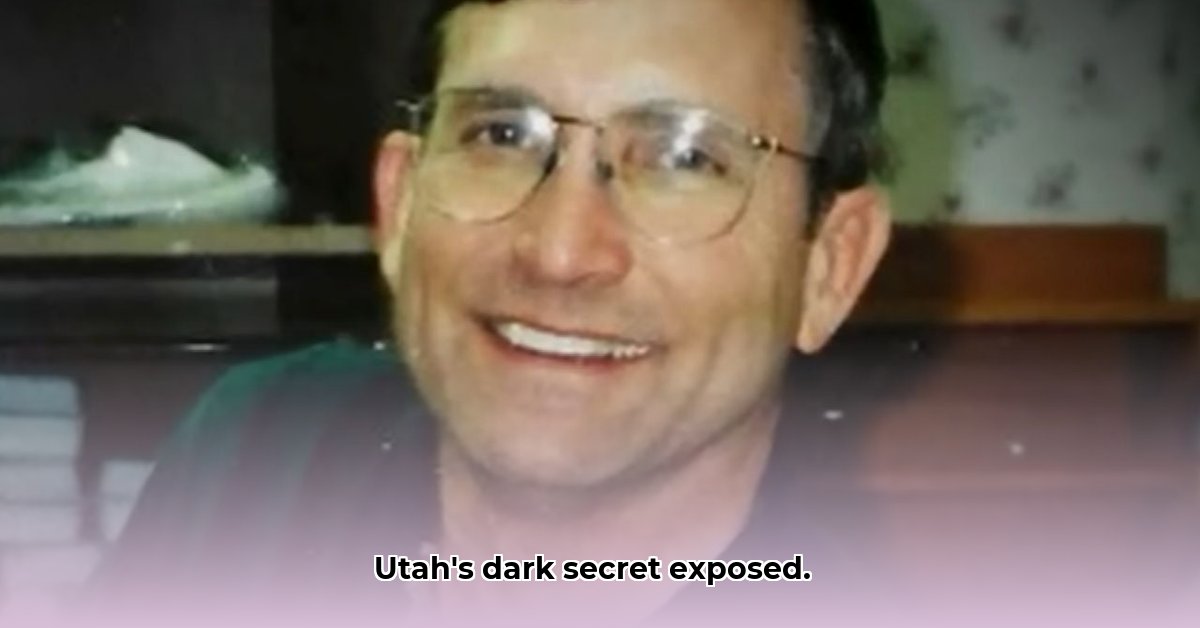
David H. Broadbent: A System's Collapse
The case of David H. Broadbent, a Utah OBGYN, transcends the actions of a single individual. It exposes a systemic failure within Utah's healthcare system and legal framework, leaving a trail of alleged victims in its wake. More than ninety women have come forward, alleging decades of sexual abuse during medical examinations. This isn't an isolated incident; it's a pattern indicative of a deeply troubling breakdown in patient safety protocols and legal accountability. The sheer volume of accusations raises critical questions about the institutions, both medical and legal, that may have failed these women. How did this happen, and what steps are being taken to prevent similar tragedies?
The allegations against Dr. Broadbent range from inappropriate touching to severe sexual assault. Each survivor's story is unique but shares a common theme: a breach of the sacred doctor-patient relationship characterized by gross misconduct. The resulting emotional and psychological trauma endured by these women is immeasurable. The persistent fight for justice underscores the systemic failures that allowed these alleged abuses to happen. But how could this happen repeatedly over such an extensive period?
A Legal Maze and Systemic Obstacles
Initially, lawsuits filed against Dr. Broadbent were wrongly categorized as simple medical malpractice cases (cases involving negligence in medical treatment, rather than intentional harm). This significant legal misclassification, a critical error in legal proceedings, became a major obstacle in bringing justice. This crucial misstep effectively shielded Dr. Broadbent from accountability for years, allowing the alleged abuse, tragically, to continue. The legal framework, intended to protect, instead inadvertently acted as a barrier to justice for these women.
This raises profound questions about the training and awareness of legal professionals concerning recognizing and prosecuting sexual assault within the context of medical malpractice. What changes are required to prevent such mischaracterizations from obstructing the path to legal recourse for victims? This necessitates a comprehensive review of legal protocols and training materials.
Institutional Responsibility: A Critical Inquiry
The extensive timeline and volume of accusations, spanning various healthcare facilities and years, raise serious questions about institutional complicity. Did these institutions fail to recognize warning signs? Did they, perhaps unintentionally, hinder the ability for victims to come forward due to systemic shortcomings or inadequate reporting mechanisms? Or, more alarmingly, were these institutions in some way complicit in enabling Dr. Broadbent's actions? These are not hypothetical questions; they demand rigorous, transparent, and independent investigations to ascertain the truth and prevent similar cases in the future. The lack of transparency only perpetuates a culture of silence that protects predators. How can we create a culture of reporting without fear of reprisal?
The Ongoing Fight for Accountability and Reform
While Dr. Broadbent has faced criminal charges and the subsequent loss of his medical license, the legal battles continue. Victims are pursuing civil lawsuits to hold him and potentially involved institutions accountable. Their ongoing pursuit transcends compensation; it's a powerful demand for systemic change to prevent future suffering. How can Utah ensure that its legal framework adequately supports and protects victims of sexual assault within the medical context?
Systemic Change: A Path to Safer Healthcare
The David H. Broadbent case is a wake-up call demanding comprehensive reform within Utah's healthcare system. While legislative changes are under consideration, this is just one component of a multifaceted solution. Healthcare institutions must implement stricter reporting mechanisms and invest heavily in comprehensive training programs to instill a culture of zero tolerance for abuse. This training must be regular and updated, including effective reporting protocols. Creating an environment where patients feel safe to report abuse without fear of reprisal is paramount. This is not about merely fixing a broken system; it’s about a fundamental cultural shift prioritizing proactive patient protection.
Key Takeaways:
- The David Broadbent case reveals a systemic failure to protect patients from sexual assault within Utah's healthcare system.
- Legal misclassifications of assault cases as medical malpractice hindered the pursuit of justice.
- Questions about institutional liability and potential complicity in enabling the alleged abuse persist.
- The ongoing fight for legal reforms emphasizes the urgent need for systemic change to create safer environments within Utah's healthcare settings.
A Call to Collective Action
The David Broadbent scandal underscores our collective responsibility to protect vulnerable individuals. This case compels lawmakers, healthcare institutions, and citizens to examine their roles and adopt decisive action. The legacy of this case must be a more just, transparent, and ultimately safer healthcare system for all. How can we ensure that lessons learned from this case lead to meaningful, lasting change?